Genetic Clues to Treatment-Resistant Depression
Polygenic dissection of treatment-resistant depression with proxy phenotypes in the UK Biobank published in Journal of Affective Disorders
For about one in three people with major depressive disorder (MDD), standard antidepressant treatments don’t work. This form, called treatment resistant depression (TRD), leaves patients struggling despite trying at least two different medications.
Our team asked: could genetics help explain who develops TRD—and even guide more personalized treatments?
Using primary-care electronic health records from 230,000 people in the UK Biobank, we identified those likely to have TRD based on their prescription history. Compared to others with depression, these individuals often had an earlier onset of depression, lower employment and education levels, and more frequent hospitalizations.
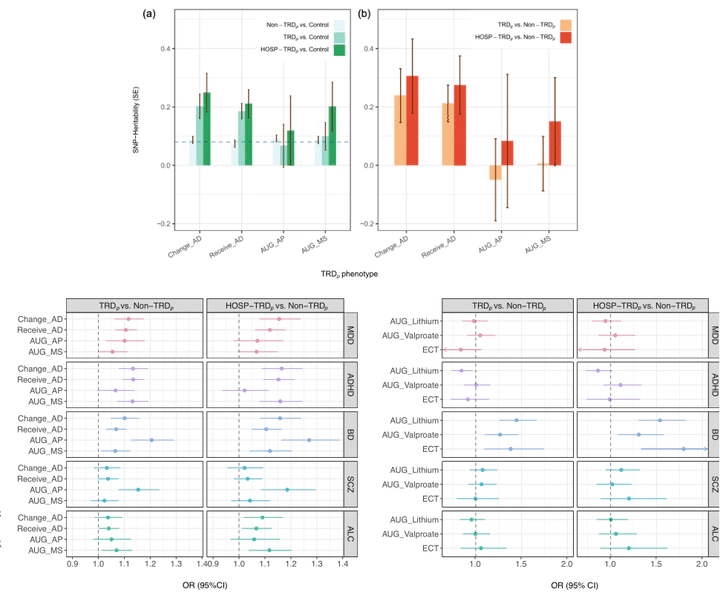
The genetic findings were clear: TRD showed a much stronger inherited component (20–30% of risk) than depression overall (~8%). People with higher polygenic risk scores (PRS) for MDD, ADHD, and bipolar disorder were more likely to switch medications or use mood stabilizers, while those with a higher genetic risk for schizophrenia specifically predicted the use of antipsychotics. Higher bipolar PRS also increased the likelihood of using electroconvulsive therapy (ECT), lithium, or valproate by 1.27–1.80 fold.
These results support that TRD has a non-trivial genetic basis and highlight the potential of PRS to uncover pharmacogenomic effects that may aid treatment options for managing TRD.
Reference:
Wang, L.-H., Shih, M.-Y., Lin, Y.-F., Kuo, P.-H., & Feng, Y. A.* (2025). Polygenic dissection of treatment-resistant depression with proxy phenotypes in the UK Biobank. Journal of Affective Disorders. https://doi.org/10.1016/j.jad.2025.04.012